In the field of Medication-Assisted Treatment, two drugs are currently on center stage: Vivitrol (naltrexone) and Suboxone (buprenorphine). In order to determine the strengths and limitations of each drug, we need to begin by defining the goals of addiction treatment. After that, we can examine how each drug meets these goals.
Treatment Goals
Most addiction treatments, whether they are medication-assisted or not, have the following four goals: to stop use, eliminate withdrawal, eliminate cravings, and, if people do use opioids, to block the ability to get high.
It’s important to point out that in the vast majority of cases, medication-assisted treatment is essential in meeting these goals. People relapse between five and nine times as often if they try abstinence. But it is rarely enough to get the job done right. The use of drugs such as Vivitrol and suboxone in medication-assisted treatment acts like a forcefield around the person using. They can protect the individual from the external triggers and internal stress, and help prevent problems from spinning out of control. In the end, however, the hope is that the person changes their external environment for the better (peers, situation, relationships) and develop strong internal reserves to manage feelings effectively. That’s real recovery. Only when the person is resilient enough to stand on their own should people consider taking down the forcefield; that is, end the medication-assisted treatment.
Vivitrol
Vivitrol is an antagonist drug. It’s been around for years as an oral table naltrexone, but has been formulated as a depot injection given once a month by a nurse or doctor. An antagonist blocks the effects of opioids on the body. Its onset is very quick and its effects last for 25 to 30 days. Additionally, Vivitrol itself doesn’t cause euphoria or withdrawal. There is no need to taper off, and once a person using gets the injection, they’re good for the next 25 to 30 days.
However, starting Vivitrol can be difficult because a person needs to be off opiates for seven days before it can be administered. So, a person has to go into withdrawal to clear out the opioids before getting the shot. Sometimes, the thought of going into withdrawal is enough for a person using to decide against the inclusion of this drug in a medication-assisted treatment. It can be really hard to stay away from opiates for that week! People often don’t make it to the shot. So, during that week the opiate-using person has to be monitored closely. This close monitoring has to be done as an inpatient in a hospital or treatment facility. Not everyone can afford to pay for such a week-long stay, and not all insurance plans cover the cost of an inpatient stay for medication-assisted treatment. Many leave before the end of the week, or relapse in the gap between discharge and getting the shot at an outpatient clinic. It would be so easy to just keep people for the 7 days and give them the shot before they leave. But it’s difficult to find an insurance plan that covers this option.
In addition, when the effects of Vivitrol begin to wear off after 25 or 30 days, there is a great risk of a relapse, or an overdose, if the person starts using again. This is because Vivitrol completely strips away any opioids from the body’s receptors. It reduces tolerance levels to that of someone that has never used opioids before. When a person stops using Vivitrol or when its effects wear off, the risk of death from an overdose is very high if the person starts using again.
It would be simple enough to administer another Vivitrol injection when the effects start wearing off. But insurance companies do not typically cover another injection until after a complete 30 days have passed since the last administration of the drug. This 25-30 day risk period needs to be prepared for and managed.
Suboxone/Buprenorphine
Buprenorphine (also known as Suboxone, Subutex, Zubsolv, or Bunavail) is given sublingually (under the tongue or against the cheek) and can be managed on an outpatient basis. It is prescribed by a trained doctor with a DEA waiver. It’s an easy training, but a lot of doctors don’t want to manage people with addictions in their office People can be started on it right away, in fact, as soon as they start withdrawing from their opiate like heroin. It’s a little tricky: take it too early and it pushes people into withdrawal. Getting started on Suboxone completely eliminates withdrawal, and at higher doses, eliminates cravings and will block heroin from affecting the cells. Because it has to be administered daily, people have to motivate themselves afresh each day. Since they are feeling good and their cravings are low, that’s not too hard. They need to see their doctor regularly, have their urines checked, and do some counseling.
On the downside, it is difficult to taper completely off from this drug. It can take months for a person using to completely get off those last few milligrams of Suboxone. It doesn’t help that the smallest dose it comes in is two milligrams – far more than the amount needed for people to start tapering off the drug. Interestingly, drug companies do not produce Suboxone pills or films in doses low enough to facilitate tapering. It makes me wonder sometimes if they do that on purpose to keep people on the drug.
Other Options
Methadone
Although this blog is really about comparing the drugs Vivitrol and Buprenorphine or Suboxone, it’s worthwhile to quickly review the attributes of one of the earliest drugs that were used in medication-assisted treatment: Methadone.
Methadone is given orally once a day in a clinic and people have to come in every day to get a dose until they get take-homes, which can be for up to four weeks. Also like Suboxone, people can start on it right away, so withdrawal is avoided. Like Vivitrol, Methadone does not cause any euphoria at steady state. However, it can be difficult to taper from Methadone, and it can cause other side effects such as weight gain or sexual side effects.
Hot off the press, there is a new buprenorphine formulation called SUBLOCADE, which is a monthly injection too. This could be a game changer. We’ll have to see.
My Preference up till November 2017: Suboxone over Vivitrol
Before two weeks ago, I favored Buprenorphine over Vivitrol (we do offer both Vivitrol and buprenorphine at Psych Garden). One reason is that there is much more research on Buprenorphine. Essentially, results show that if you go with the abstinence-only treatment for heroin addiction, there is a zero to five percent success rate. People who are highly dedicated will succeed if they are very lucky and given a lot of support and a lot of time. But for Buprenorphine, eighty to ninety percent of the people will become opioid-free. This percentage rate goes down to about 50 or 60 percent in certain problematic populations in the United States. Typically this involves challenging outpatient situations with concerns about insurance coverage and poverty, as well as difficulty in engaging patients and keeping them compliant. Nevertheless, the overall rate of a person using becoming opioid-free is much better for Buprenorphine and well-established. Naltrexone, on the other hand, as a pill, had a long unsuccessful history, and, as a depot injection, was only tested in Russia with a limited population.
I was skeptical, too, because I believed that, while buprenorphine NORMALIZED stress hormone abnormalities so central to addiction, naltrexone should, theoretically, worsen that. I thought that would result in Naltrexone or Vivitrol worsening stress in people with a history of trauma or anxiety disorders. I was also worried that Vivitrol would result in higher rates of overdose, because (as already stated above) it completely strips away any opioids from the body’s receptors, and reduces tolerance to that of a person who has never used opioids before. So, when the people stop using Naltrexone or Suboxone, the risk of death would be very high.
My Current Preference: Vivitrol over Buprenorphine
A couple of studies have recently come out in The Lancet that has shifted my preference towards using Vivitrol over Buprenorphine. One study screened about seven hundred people that they divided into two groups, one using Vivitrol and the other using Buprenorphine. They followed them for two years.
There were way more drop-outs in the Vivitrol group in the first phase of treatment, for the reasons I discussed above: they couldn’t make it the seven days till they could get the injection, even though they were in inpatient detox. There were seventy-nine induction failures to Vivitrol, and there only seventeen induction failures in Buprenorphine.
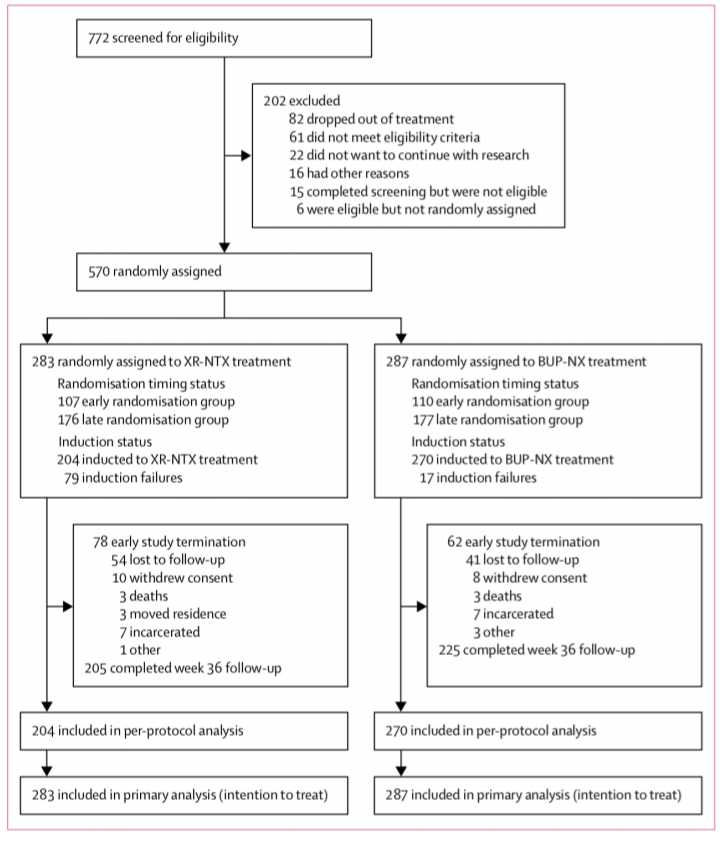
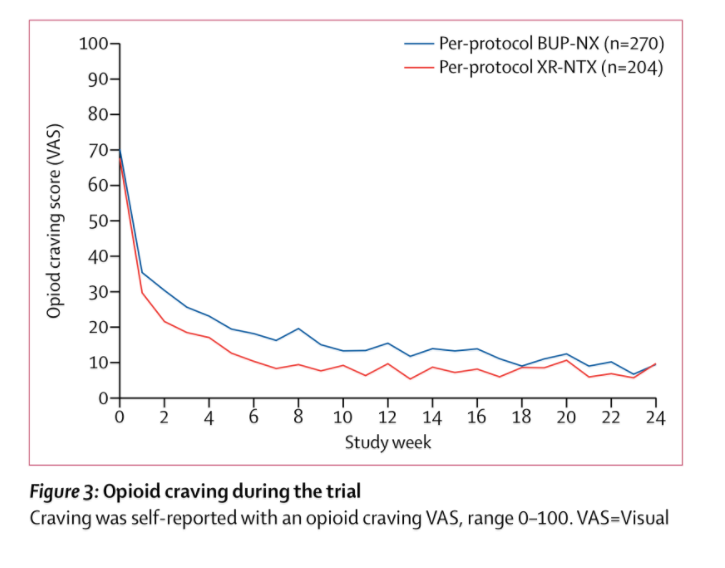
Once people are on the drug though, both groups did as well as the other. Seventy-eight terminated early from Vivitrol, and sixty-two from Suboxone, and there were a similar number of deaths and incarcerations in either group. The average Suboxone dose was around 16mg. Relapse was measured realistically: either seven consecutive days or four consecutive weeks of positive urine tests.
Summary
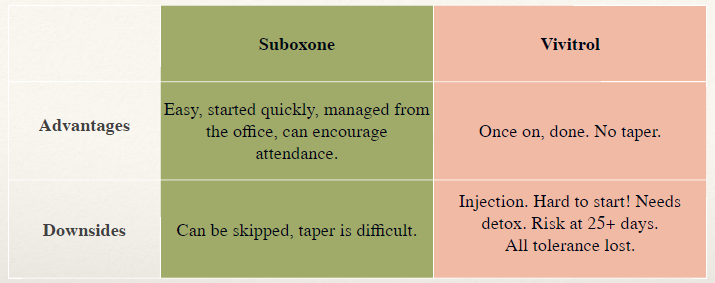
In summary, Suboxone has the following going for it: it’s easy to start as it doesn’t require a withdrawal period, distribution can be managed in an office, and so people can be encouraged to engage in therapies. There are downsides to Suboxone as well: clients can easily decide to skip a dose (or more) and it is difficult to taper from Suboxone – especially those last few milligrams. And, the drug can be shared and diverted.
Vivitrol’s advantages include the following: it is administered as an injection that lasts up to 30 days so once a person is on it, they’re good for that length of time (no daily visits), and there is no need to taper from Vivitrol. The main disadvantage to Vivitrol is the required seven-day detox before the drug can be administered. This has to be managed as an inpatient stay, which can be expensive (since not many insurance plans cover this) and impractical for most people. Additionally, the drug wears off around 25 to 28 days, but insurance will only cover another shot after 30 days, so there’s a higher risk of a relapse towards the end of the effective period of the drug. There can even be the danger of an overdose if the patient starts using again during this time since all tolerance is lost when a person is started on Vivitrol – though surprisingly, in the study discussed here, the overdose rates were not different from people prescribed buprenorphine. It remains to be seen whether Vivitrol is a good choice for patients with added psychiatric issues and/or trauma. However, neither I nor any colleagues I’ve spoken with have seen it as a negative effect on this population.There has been no evidence of increased anxiety on people that are using Vivitrol.
In terms of my practice, I’ll be more likely to use Vivitrol now, although every treatment protocol is based on an individual’s needs and situation. A lot of focus and support needs to be given during the seven-day detox period because the patient is extremely vulnerable at this stage. Close professional supervision and guidance are needed at this point. Additionally, the client’s family, colleagues, and community should ideally be engaged and rallying behind them at this point. The client should also be closely supervised and followed when the drug’s effectivity begins to wear off after 25-30 days when the risk of a relapse or an overdose is greatest.
I urge you not to be persuaded by nonsense about some moral superiority of abstinence-based treatment, or that medication-assisted treatment is just substituting one addictive substance for another. People develop an opioid addiction over many years of compulsive use, and you are not causing any further addiction by using Suboxone or Vivitrol, so please discard that notion. That’s just stigma and it kills people.
Instead, treatment needs to be individualized. It should be based on a patient’s preference, whether the person can keep away from opioids for seven days, and other personal considerations. There should be more than one option since a person does not always do well on the first drug. There’s not just one treatment for cancer or an infection. Some people are better suited to a different kind of structure and the treatment might be an outpatient program or clinic, where they have to go every day or every few weeks. Addiction treatment centers on the person using, and the drugs, methods, professional and personal supports that best aid them in their quest to live lives that are independent of drugs.

